Abstract
This is a case of a pediatric patient who presented with a sudden onset of right abducens nerve palsy with contralateral hemiplegia with no facial paralysis. With the constellation of symptoms aided by the presence of enhancing pontine mass on magnetic resonance imaging, the presence of diffuse intrinsic pontine glioma (DIPG) was presumed to have caused the findings consistent with the common type of Raymond syndrome.
Author Contributions
Academic Editor: Zheng Jiang, Johns Hopkins University School of Medicine
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Danica Tomas-Esteban, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Raymond syndrome is one of the ocular motor clinical syndromes that is mainly characterized by ipsilateral abducens nerve palsy and contralateral hemiparesis1 or hemiplegia.2 The lesion in these cases affects the ventromedial pons where the abducens nerve fascicle and nondecussated corticofacial and corticospinal tract are located.1There are two syndrome types depending on the structures involved: 1. classic type, involving the ipsilateral abducens fascicle, undecussated corticofacial and corticospinal fibers, and 2. common type, caused by a lesion involving the ipsilateral abducens fascicle and non-decussated corticospinal while sparing the corticofacial fibers.3
The objective of this paper is to report a case of a pediatric patient with medial deviation of the right eye associated with left sided hemiplegia, diagnosed as a case of Raymond Syndrome (common type), which is an extremely rare neurologic condition among pediatric patients.
Case Report
This is a case of a six-year old, female, brought in due to sudden onset, painless, inward deviation of the right eye three months prior to consult. It was progressive and associated with left sided weakness; the guardian denied any history of trauma, previous occurrence, variability nor other systemic symptoms such as fever or weight loss.
On clinical examination, patient was conscious and alert, not in pain nor in respiratory distress. Patient was noted to be dragging her right leg on walking with an inwardly folded right arm. Best corrected visual acuity was 6/7.5 on both eyes with a refraction of +1.00 ( ) -0.50 x 180 on the right and + 1.50 on the left. Anterior and posterior segments of the eye including the optic nerves were unremarkable. A 30-prism diopter esotropia was noted on the right eye. There was -4 limitation on abduction, and on superolateral and inferolateral movement of the right eye on version testing. Abduction deficit of the right eye persisted on duction testing and on doll’s head manuever. A left sided hemiplegia was noted, and the rest of the neurologic findings were normal, with no noted facial asymmetry or weakness. With the constellation of findings, Raymond Syndrome was the primary consideration.
Cranial MRI with contrast was done, revealing a right pontine mass with features of glioma typical of a diffuse intrinsic type exhibiting T1 hypointensities, T2 hyperintensities involving majority of the pons with associated signal changes.4Hence, patient was diagnosed with Raymond Syndrome probably secondary to a presumed pontine glioma, Right. Patient was referred for evaluation and co-management with Neurosurgery and Pediatric Neurology services. Patient subsequently underwent radiotherapy.
Red arrow: Peripherally enhancing 2.6 x 4.1 x 2.8 cm lobulated mass centered on the right tegmentum of the pons, exhibiting hyperintensity (and hypointensity in T1 weighted images, not shown). Mass renders the pons enlarged and displaces the rest of the pontine parenchyma peripherally. Green arrow: Effacement of bilateral cerebellopontine angle. Yellow arrow: Mild compression on the 4th ventricle. Blue arrow: Small similar looking lesions at medulla oblongata. (Figure 1, Figure 2)
Figure 1.Nine gaze photo showing an inwardly deviated right eye with a full limitation on superolateral and inferolateral gazes.
Figure 2.T2 Weighted cranial magnetic resonance imaging sagittal (a) and axial (b) cuts.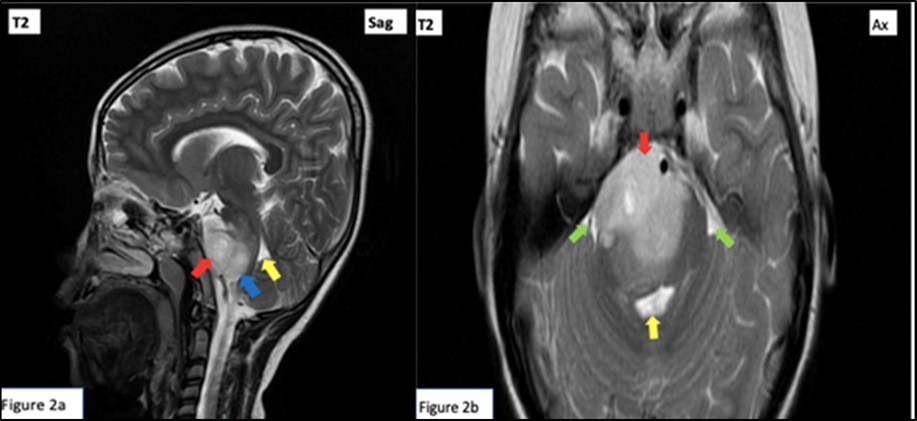
Discussion
An injury to the ventral pons results to either Raymond and Millard-Gubler syndromes; each can be differentiated generally by the affectation to the facial nerve with Raymond presenting as alternating ipsilateral abducens weakness with contralateral hemiplegia while Millard-Gubler manifesting with ipsilateral facial paresis. However, with the advancement in cranial imaging, neuroanatomical correlation has been widely explored and it was found out that contralateral central facial paresis may also occur at the pontine base as what is seen in the classic type of Raymond syndrome. 3
In general, few cases of Raymond syndrome had been reported 4, 9, mainly of the common type and less of the classic type3. Furthermore, pure Raymond syndrome is an extremely rare neurologic disorder as many structures present along the abducens nerve fascicle may be affected.4
Raymond syndrome is a posterior circulatory stroke syndrome11 mostly affecting adults, however, may also be seen in children. An abducens nerve paresis in a young child raises the suspicion for Diffuse Intrinsic Pontine Glioma (DIPG) since it is regarded as a highly sensitive predictor 7 and magnetic resonance imaging is usually diagnostic.8 DIPG, histologically characterized as astrocytoma, is a fatal brain tumor, accounting for 10-20% in affected pediatric population.10. In this case, Raymond Syndrome brought about by DIPG was a primary consideration on the basis of the presentation of sudden onset of sixth nerve palsy in a young patient supported by the typical radiologic findings consistent with glioma. Furthermore, surgical debulking is a challenge because of its eloquent brainstem location, making radiation therapy the only proven treatment in prolonging progression-free survival.5
Conclusion
This is a case report of the common type of Raymond Syndrome in a pediatric patient, manifested as ipsilateral abducens nerve palsy with contralateral hemiparesis, without an accompanying contralateral facial paresis brought about by a large pontine mass.
References
- 1.N R Miller, W F Hoyt, F B Walsh. (2005) . Chapter 40 Cerebrovaascular disease. InWalsh and Hoyt's clinical neuro-ophthalmology(6th Edition). table, Lippincott Williams & Wilkins 2.
- 2.Toppel V L. (1967) Strabismus paralyticus als Teiler-scheinung eines doppelseitigen Raymond- Syndroms. , KlinMonatsblAugenheilkd 151, 663-72.
- 3.N G Zaorsky, Luo J J. (2012) A case of classic raymond syndrome. Case reports in neurological medicine. 583123.
- 4.Satake M, Kira J, Yamada T, Kobayashi T. (1995) Raymond syndrome (alternating abducent hemiplegia) caused by a small haematoma at the medial pontomedullary junction. Journal of neurology, neurosurgery, and psychiatry. 58(2), 261.
- 5.R K Mathew, J T Rutka. (2018) Diffuse Intrinsic Pontine Glioma : Clinical Features, Molecular Genetics, and Novel Targeted Therapeutics. , Journal of Korean Neurosurgical Society 61(3), 343-351.
- 6.Sciacca S, Lynch J, Davagnanam I, Barker R Midbrain, Pons et al. (2019) . , Anatomy and Syndromes. Radiographics 39(4), 1110-1125.
- 7.Fisher P G, Breiter S N, Carson B S, Wharam M D, Williams J A et al. (2000) A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as dis- tinct entities. , Cancer 89, 1569-1576.
- 8.Freeman C R. (1999) Perilongo G: Chemotherapy for brain stem gliomas. , Childs Nerv Syst 15, 545-553.
- 9.Khan M, Naveed S, Haider I, Humayun M, Khan A. (2017) Classic Raymond Syndrome. J Coll Physicians Surg Pak. 27(3), 185-186.
Cited by (1)
- 1.Ground Marcus, Punter Martin N M, Rosemergy Ian, 2023, Pontine ischaemic stroke syndromes, Practical Neurology, 23(6), 501, 10.1136/pn-2023-003782
